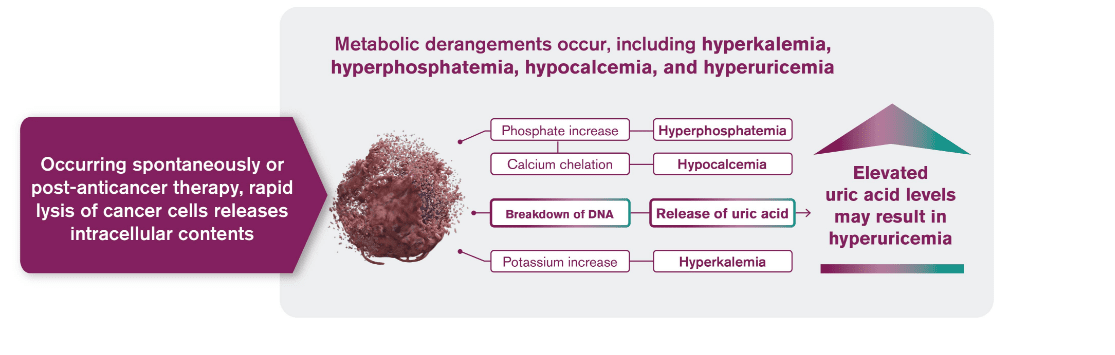
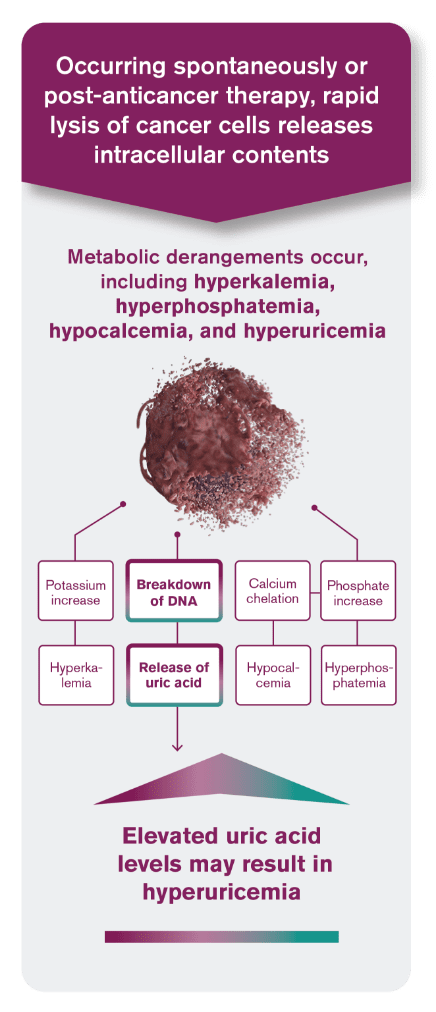
Tumor lysis syndrome (TLS) is caused by a massive release of intracellular contents into peripheral blood that results in metabolic derangements1
Hyperuricemia
Hyperkalemia
Hyperphosphatemia
Hypocalcemia
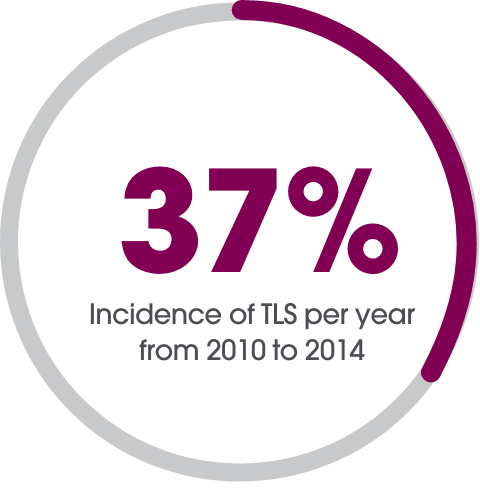
TLS is prevalent in hematologic malignancies with1:
- High proliferative rate
- Large cellular burden
- High sensitivity to chemotherapy or cytolytic antibody therapy
TLS occurs spontaneously or in response to anticancer therapy, usually 12 to 72 hours after the start of therapy1,2

TLS associated with hyperuricemia may lead to serious clinical complications2

EXPERT REVIEW VIDEO
Watch Dr. Ali McBride explain the relationship between uric acid levels and the risk of TLS in patients with hematologic malignancies.
Are your patients at higher risk for TLS than you think?
Use this Risk Assessment Tool to help you identify patients who may be at risk for TLS
VISIT NOW
ALL=acute lymphoblastic leukemia; CLL=chronic lymphocytic leukemia; NCCN=National Comprehensive Cancer Network; SLL=small lymphocytic lymphoma.
References: 1. Cortes J, Moore JO, Maziarz RT, et al. Control of plasma uric acid in adults at risk for tumor lysis syndrome: efficacy and safety of rasburicase alone and rasburicase followed by allopurinol compared with allopurinol alone—results of a multicenter phase III study. J Clin Oncol. 2010;28(27):4207-4213. 2. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas. V.4.2022. ©National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed August 26, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 3. Howard SC, Jones DP, Pui CH. The tumor lysis syndrome. N Engl J Med. 2011;364(19):1844-1854. 4. Edeani A, Shirali A. Chapter 4: Tumor Lysis Syndrome. Onco-Nephrology Curriculum. American Society of Nephrology. 2016. https://www.asn-online.org/education/distancelearning/curricula/onco/Chapter4.pdf. Accessed August 26, 2020. 5. Pathak R, Giri S, Aryal M. Recent trends in the incidence and outcomes of tumor lysis syndrome in hematological malignancies: Data from 2010-2014 National Inpatient Sample. Blood. 2017;130:3390. 6. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma. V.3.2022 ©National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed August 26, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 7. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Acute Lymphoblastic Leukemia. V.3.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed August 26, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.